A summary of each CBD Stage/Postgraduate Year
PGY 1 – Transition to Discipline (TTD):
This 9 block stage offers a comprehensive clinical experience, in order to round-out physician training post clinical clerkship. The rotations serve to enhance clinical material relevant to future training in Diagnostic Radiology. The rotations are based at one of the four city hospitals.
The two overriding broad objectives of this clinical year are:
- To provide the opportunity to experience clinical medicine and broaden your medical background.
- To gain a better understanding of the relevance of diagnostic imaging for a variety of medical disciplines.
The TTD stage is 9 blocks long and consists of rotations through a number of core medical specialties. Currently, the year consists of:
| ROTATION | DURATION |
| General Surgery | 2 blocks |
| Internal Medicine | 2 blocks |
| Emergency Medicine | 2 blocks |
| Anatomical Pathology | 1 block |
| Neurology | 1 block |
| Pediatrics | 1 block |
| Intro to Radiology | 1 block |
The final two block blocks of TTD are dedicated to Imaging Anatomy and an introduction to the basics of medical imaging. The overall aim is to review and enhance anatomical knowledge, as it applies to diagnostic imaging. The major focus is on cross-sectional imaging anatomy with ultrasound and CT. The rotation format consists of small group learning sessions with Anatomists in the anatomy lab, as well as with ultrasound faculty members and technologists. In addition, a substantial component of the rotation includes self-directed independent learning, in order to achieve the outlined anatomical objectives. Residents also commence radiology “buddy call” during this time, exposing them to cross-sectional anatomy in practice. As well, this serves as an introduction and orientation to “on-call” in radiology.

PGY 1/2 – FOUNDATIONS of DISCIPLINE:
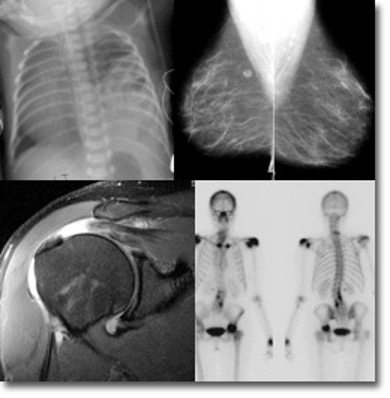
The Foundations stage is 8 blocks long and consists of short introductory rotations in Emergency Radiology, Pediatrics, Chest, MSK, Neuroradiology and CT. These rotations are designed to introduce the resident to areas of imaging frequently encountered on-call. During this time, the resident will learn radiology terminology, as well as how to structure a report. A key component of this introductory time includes learning the basics of PACS, image manipulation and communication skills.
The current blocks consist of:
1. Neuroradiology
2. Pediatrics
3. ER/trauma
4. Chest
5. MSK
6. Body CT
7. CT Intro
8. US Intro

PGY 2-5 – CORE of DISCIPLINE:
This stage is split into Juniour and Senior Core substages, each which is 20 blocks long. It is focused on the core competences of radiology. During this time, you will also participate in the after-hours independent call reporting responsibilities.
Residents attend the 4-week Radiology/Pathology course at the ACR Institute for Radiologic Pathology (AIRP), in person in Washington D.C or virtually (usually during PGY 4). Financial support is provided to attend this course. Residents will also complete a community elective block to experience radiology outside of the academic setting. The typical rotations design for this year includes:
Junior blocks: Adult GI, Chest (x2), MSK, US (x2), CT (x2), Peds body, Nuclear Medicine, MRI, Neuro CT, Neuro MR, IR (x2), Cardiac, Breast (x2), OB US (x2)
Senior blocks: CT (x2), Chest, Adult GI, MSK (x2), MRI (x2), Peds MSK, Peds Neuro, IR, Neuro MR, Nuclear Medicine (x2), Community/IHF rotation, AIRP, Elective (x2), Breast (x2)
PGY 5 – TRANSITION to PRACTICE:
This stage is 6 blocks long and allows the resident to focus on fine-tuning knowledge in areas of interest and address educational gaps. This is intended to round-out senior resident consultancy skills, as well as to serve as a foundation for review of content relevant for independent practice or fellowships. Residents are able to provide significant input into their rotation design, including order of rotations, as well as choice of site for placement.
This year includes 4 “Junior Staff” rotations and 2 elective rotations. During these rotations, residents can tailor their rotation design to those areas that best suit their personal learning objectives and future career direction. This permits the PGY 5 resident flexibility in designing their year, best suited to their educational needs. These rotations serve to consolidate consultancy skills in Diagnostic Imaging, as they permit graded responsibility and independent reporting, fostering a “ready for practice” model by completion of the PGY 5 year. During these blocks, the senior resident target is to carry the responsibilities and workload of a Junior Staff Radiologist. It is during these rotations that our residents are able to review core material, by “on the job” exposure to important imaging material, including plain radiography
Our program design adheres to the Royal College of Physicians and Surgeons of Canada National Standards for Diagnostic Radiology. For more specific information, visit the Royal College website: Home (royalcollege.ca)
Graded Resident Responsibilities:
There is a hierarchical structure to the learning process which:
- Allows the residents responsibility commensurate with training and ability.
- Permits different levels of teaching and learning through teaching.
PGY 2 and 3 residents are the most closely supervised. They review imaging studies on their own and then each exam is reviewed with them by the attending staff person. The resident issues the report, which is then checked by the supervising staff person. If the Competence Committee and rotation supervisor are satisfied with a resident’s performance, then by their PGY 5 year, they can review cases and report independently. Junior residents learn procedures under close supervision of a staff person, and as they become more senior and skilled, they graduate to performing procedures on their own, with supervision as appropriate.
All residents have a responsibility for teaching each other, residents from clinical specialties (for example, during informal consultations in the department or on working rounds), clinicians, technologists, and nursing staff.
The most senior resident in the hospital at any one time has some administrative responsibilities. They function to assist in the supervision and teaching of junior house staff and clinical clerks, organize and ensure the maintenance of educational rounds and other educational events. They also assist in liaison between resident staff and consultant staff
On-Call Duties
In their PGY-2 year, residents perform on-call duties from the beginning of the program year. For the first 5 to 6 months, PGY-2 residents are paired with more senior residents, during which they transition from a largely observational role to the primary contact person, or “first call” resident. Following this orientation period of “double-call”, most residents are capable of independent call, with fellow/staff back-up.
Our program has designed a “Call Centre” model for after-hours imaging coverage. Three residents are on-call for the city, covering requests from all four teaching hospital sites. They are both housed at the Hamilton General site and cover the Juravinski, MUMC and St. Joseph’s Hospital sites remotely. This model facilitates a more team-based approach to call in radiology, as no resident is on alone. In addition, it permits a more equal distribution of the on-call workload. The model has been well-received by the residents and was designed with input from the resident body. There is no interventional call for residents, but they can be involved if they are interested.
The on-call Staff Radiologists are always available to consult by phone or come in as needed.
Graded Resident Responsibility & On-Call Duties:
There is a hierarchical structure to the learning process which:
- Allows the residents responsibility commensurate with training and ability.
- Permits different levels of teaching and learning through teaching.
PGY 2 and 3 residents are the most closely supervised. They review imaging studies on their own and then each exam is reviewed with them by the attending staff person. The resident issues the report, which is then checked by the supervising staff person. If the Education Committee and rotation supervisor are satisfied with a resident’s performance, then by their PGY 5 year, they can review cases and report independently. Junior residents learn procedures under close supervision of a staff person, and as they become more senior and skilled, they graduate to performing procedures on their own, with supervision as appropriate.
All residents have a responsibility for teaching each other, residents from clinical specialties (for example, during informal consultations in the department or on working rounds), clinicians, technologists, and nursing staff.
The most senior resident in the hospital at any one time has some administrative responsibilities. They function to assist in the supervision and teaching of junior housestaff and clinical clerks, organize and ensure the maintenance of educational rounds and other educational events. They also assist in liaison between resident staff and consultant staff.
On-Call Duties
In their PGY-2 year, residents perform on-call duties from the beginning of the program year. For the first 5 to 6 months, PGY-2 residents are paired with more senior residents, during which they transition from a largely observational role to the primary contact person, or “first call” resident. Following this orientation period of “double-call”, most residents are capable of independent call, with fellow or staff back-up.
Our program has designed a “Call Centre” model for after-hours imaging coverage. Two residents are on-call for the city, covering requests from all four teaching hospital sites. They are both housed at the Hamilton General site and cover the Juravinski, MUMC and St. Joseph’s Hospital sites remotely. This model facilitates a more team-based approach to call in radiology, as no resident is on alone. In addition, it permits a more equal distribution of the on-call workload. The model has been well-received by the residents and was designed with input from the resident body. There is no interventional call for residents, but they can be involved if they are interested.
At the General Hospital Campus, the resident is an integral member of the Trauma Team.
The on-call Staff Radiologists are always available to consult by phone or come in as needed.
